When Everything Is Under Pressure: How Behavioral Health Leaders Are Rebuilding Stability for 2026

Behavioral health leaders are heading into 2026 under sustained and compounding pressure. Workforce strain continues to weigh heavily on teams, regulatory requirements keep shifting, and payer dynamics feel less predictable than they did even a year ago. With expectations around access, outcomes, and long-term sustainability continue to rise, leaders like you are feeling boxed in, with little room for missteps and less tolerance for inefficiency.
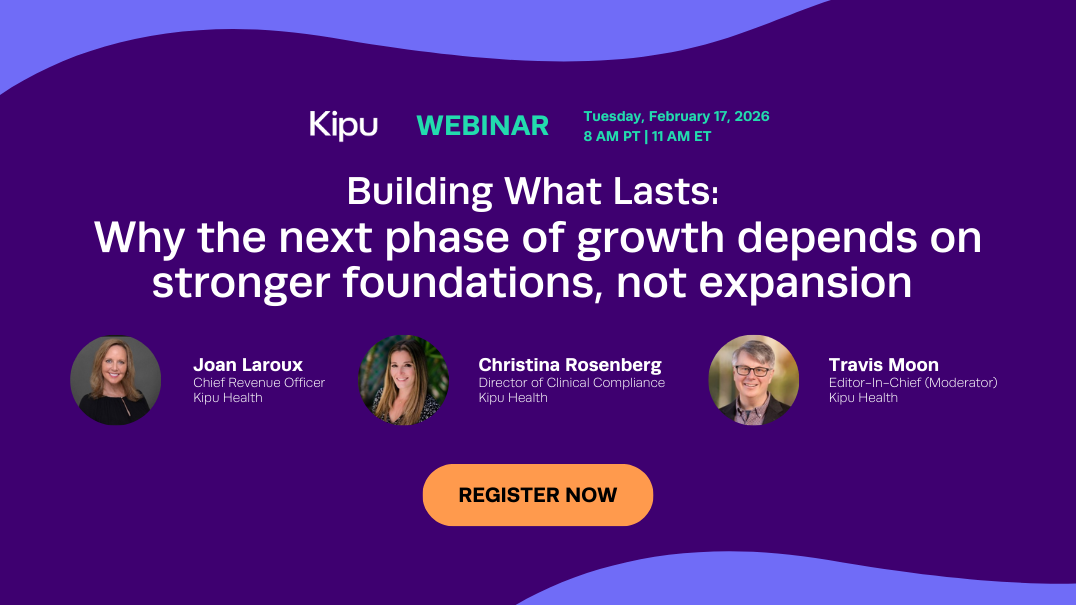
What stood out most in our recent leadership webinar, Under Pressure: A 2026 Leadership Guide to Workforce Stability, AI, and Regulatory Change, highlighted how clearly the conversation has shifted toward designing for resilience. We’re seeing leaders increasingly investing in durable systems designed to hold under pressure and support long-term stability. As Kipu’s CEO, Carina Edwards, shared in the webinar, “Having your data sound, having your foundation built, not trying to splice insights from across the organization — that’s how organizations stay stable in uncertain times.”
Across organizations of all sizes, leaders are arriving at similar conclusions through very different paths. Regardless of size, setting, and service mix, the emerging operational decisions are remarkably consistent, and they offer a practical blueprint for navigating what comes next.
Workforce stability starts with operational relief
Workforce conversations often start with hiring, but leaders are finding that stability is shaped much earlier and much closer to day-to-day operations. Burnout is being created by workflows that demand too much time, systems that ask clinicians to translate their work twice, and processes that push essential tasks into evenings and weekends.
A clear early signal of workforce risk shows up in operational drag. Documentation that consistently runs long and administrative work that spills beyond clinical hours create a steady accumulation of fatigue that leaders can see long before turnover appears.
Organizations seeing improvement are focusing on removing that drag. They start by identifying the few workflows that absorb the most clinician time and attention. As Kipu CEO Carina Edwards noted during the discussion, “It’s process, not technology, that should drive the changes.”
In practice, leaders are rethinking how clinical work actually moves through the organization. Assessments are being reshaped to reflect real clinical judgment rather than rigid templates, and documentation is happening closer to the moment of care, while context and nuance are still intact. Clinical, compliance, and billing teams are aligning around shared expectations, allowing clinicians to document once and trust that their work will support quality, compliance, and reimbursement without repeated handoffs or rework.
That shift changes the day-to-day experience in meaningful ways. Clinicians regain time and mental bandwidth, not by rushing through care, but by removing friction that never added value in the first place. Workdays become more predictable. Leaders gain confidence that documentation reflects the care delivered and holds up under scrutiny. Over time, those improvements strengthen retention, stabilize teams, and help organizations sustain the pace and complexity of behavioral health care.
AI works when it solves real problems
AI adoption continues to rise, but the strongest results are coming from leaders who treat it as an operational tool, not a strategy headline.
The pattern is consistent:
- Start with a clear use case
- Measure the baseline
- Pilot with a small group
- Build internal champions
- Expand once results are visible
Organizations that follow this path are seeing tangible results that show up quickly in daily operations. Documentation takes less time and feels less burdensome, new clinicians reach confidence faster, and notes become more consistent and clinically useful. In some cases, those improvements are also strengthening reimbursement performance by reducing gaps and omissions that lead to denials or delays.
Over time, a quieter benefit begins to emerge. As AI becomes embedded in everyday workflows, it reinforces learning and consistency across teams. Clinicians receive feedback in context, expectations become easier to interpret and apply, and quality improves naturally as part of the work, rather than through additional oversight or review layers.
Compliance belongs upstream
Regulatory anxiety ranked high again this year, particularly around funding risk and payer scrutiny. Confidence in payer negotiations has softened. Smaller organizations feel especially exposed.
What’s changing is how leaders are addressing that risk. Rather than treating compliance as an after-the-fact review, more organizations are building it directly into clinical and operational workflows.
When documentation aligns with payer requirements from the start, audits become less disruptive. When quality checks happen before a note is signed, teams spend less time fixing issues downstream. Compliance stops being a binder on a shelf and starts functioning as infrastructure.
This shift also improves collaboration between clinical and revenue cycle teams. When both groups work from shared expectations and shared data, friction decreases and outcomes improve.
Growth is getting more disciplined
Another clear signal from the conversation is that growth in 2026 carries far higher stakes than it did in previous years. Leaders are no longer chasing scale for its own sake. They are asking a more consequential question: which forms of growth actually make the organization stronger rather than more fragile?
Across the webinar, executives described a shift toward growth that deepens capability instead of spreading resources thin. Service line extension and level-of-care expansion are being used to keep patients engaged longer, deliver more complete care, and reduce avoidable handoffs that erode both outcomes and revenue. Growth disconnected from operational readiness simply amplifies existing weaknesses.
That reality is forcing a harder look at integration. Referral intake, clinical delivery, outcomes tracking, and reimbursement performance are being treated as a single continuum rather than a set of adjacent systems. Leaders shared how mapping workflows end to end has helped expose where patients fall through the cracks, where data breaks down, and where financial risk quietly accumulates.
For organizations that do this work, the payoff extends well beyond clarity. Leaders gain the ability to invest with confidence, expand services that align with patient need, and make growth decisions grounded in evidence rather than instinct. In a year defined by constraint, that kind of disciplined growth becomes a competitive advantage rather than a liability.
Intentional design beats reactive change
The common thread across all of this is intentionality.
The leaders who feel most prepared are not trying to fix everything at once. They are choosing where to focus, aligning teams around that choice, and using technology to support the work rather than reshape it overnight. They are also leaning on partners, asking hard questions about workflows, and being willing to redesign processes that no longer serve them.
Pressure is not going away. But pressure does not have to mean instability. With the right foundations in place, it can become a catalyst for smarter systems, healthier teams, and more sustainable care delivery.
That is the opportunity in front of the behavioral health community right now. And the leaders who embrace it will shape what the next decade looks like.
Want to see how Kipu can help your organization?
Recent Posts
Rely on Kipu to keep you ahead of change.
Subscribe to Kipu for behavioral health news, updates, community celebration, and product announcements.